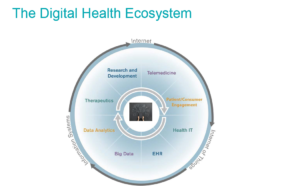
Join McDermott next Wednesday for a live webinar on the unique considerations in developing and procuring AI solutions for digital health applications from the perspective of various stakeholders. We will discuss the legal issues and strategies surrounding:
- Research and data mapping essential to the development and validation of AI technologies
- Protecting and maintaining intellectual property rights in AI solutions
- Technology development
- Risk management and mitigation for various contractual arrangements, including contracts with customers, vendors and users
We will also focus on the trends in US law for AI solutions in the digital health space, and present actionable advice that will help you develop an effective strategy for developing and procuring AI solutions for digital health applications.
Developing and Procuring Digital Health AI Solutions: Advice for Developers, Purchasers and Vendors
Wednesday, June 13, 2018 | 11:00 am CT | 12:00 pm ET
Register Here
read more

 Subscribe
Subscribe