The idea of keeping people healthy at home has become more relevant than ever during the COVID-19 public health emergency. The expansion of telemedicine during the pandemic is expected to serve as a catalyst that will permanently change the way providers deliver care and patients engage with their health. Joined by leaders from Cricket Health, Livongo and BehaVR, we discussed factors driving the shift towards expanding digital delivery of healthcare services and the challenges – technological, regulatory and cultural – that impact such expansion. Click here to listen to the webinar recording, and read on for highlights from the program.
To learn more about the “Around the Corner” webinar series and attend an upcoming program, click here.
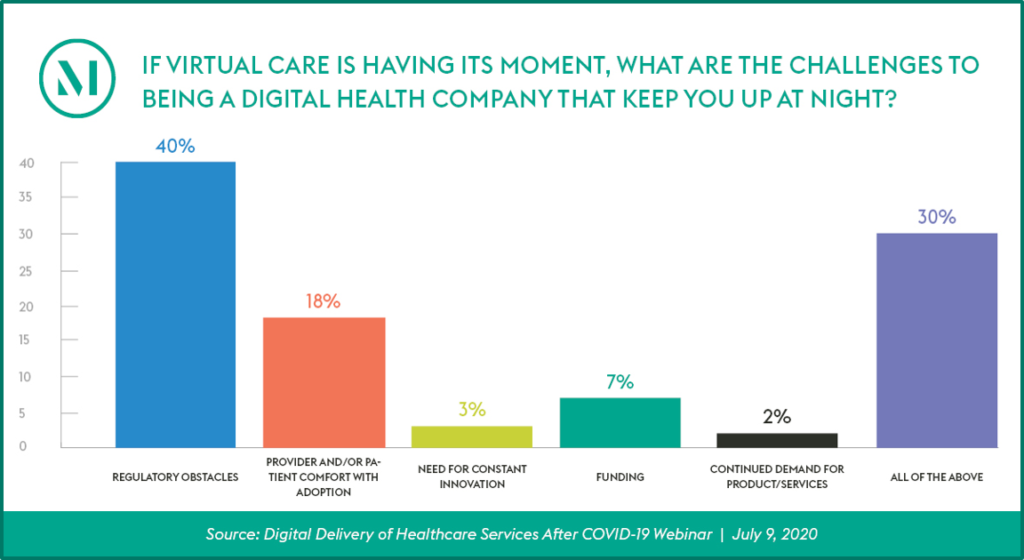
Audience Perspective
Program Insights
- A redoubled focus on preventative care will be key to bring about effective digital health delivery. The current US healthcare delivery system, built mainly on reimbursable, episodic care, is consistently indicted for being a “sick care” system, not a “healthcare” system. Patients, especially patients with chronic healthcare conditions such as diabetes, hypertension, behavioral health and acute kidney disease, need constant, real-time support and guidance, and need their providers to have access to accurate, actionable information to manage these conditions between real-time encounters. Digital health will play a vital role in this effort.
- New care modalities open the door to structural changes, which will need to keep pace with the healthcare system. How emerging care modalities are integrated into and affect the healthcare system are still in development, and raise a variety of concerns, from staffing and technology needs to privacy safeguards. As the healthcare system adapts to these changes, the regulations that govern care delivery, licensing, and accreditation will need to adjust as well.
- Positive regulatory changes have been implemented during the pendency of the national pandemic emergency, but those or similar regulatory changes must continue, and gain momentum and reach, for lasting changes to occur. The actions taken by regulators during the COVID-19 public health emergency show that the government can swiftly respond to new ideas and paths to care. However, these actions are temporary, and it will take time to implement lasting change. While there is an appetite to make some common-sense changes permanent, other areas, such as multi-state professional licensing, will likely take more time due to their complexity.
- Reimbursement models based around episodic care are a major hurdle to the adoption of on-going remote monitoring and other digital health tools. Panelists agreed that when reimbursement structures are aligned with value-based care, such that providers are reimbursed for the outcomes and on-going care management they provide, digital health tools become a critical part of the provider’s toolbox. In the meantime, digital health companies that have outcomes data to effectively compete in alternative value-based pricing arrangements will have an advantage. Companies will want to consider developing sufficient and credible evidence with respect to value as they would with respect to the safety and effectiveness of their technology.
- Both patients and providers will need to reimagine the healthcare delivery system and patient experience to support digital health adoption. Virtual healthcare delivery is a real-time, all-the-time, multi-tool, multi-provider endeavor. It may be difficult for patients to conceive of what their healthcare could look like. Overcoming this patient trepidation is critical, but if successful, panelists reported that patients become quickly committed and invested in their healthcare. Digital health companies and adopters can help smooth this transition by carefully considering the nuts and bolts of the patient experience – walking the technology through the patient’s steps – to anticipate gaps, ambiguities or concerns – and proactively address them.
- Digital health tools, with a focus on remote monitoring and virtual care, create the 24/7 healthcare delivery necessary to sustain the positive outcomes and quality of life for patients with chronic conditions. Absent such tools, patients will struggle to navigate their conditions. Stabilizing and monitoring the health of chronically ill patients from the safety of their own homes whenever possible is essential to minimizing disease transmission and risks to these patients, who are more vulnerable to the virus and more likely to experience worse outcomes.
- Digital therapeutics can advance digital health delivery. Many of the digital health tools help monitor, analyze, and support healthcare—they are care management tools and perhaps digital diagnostics. Our panelists, however, also noted that digital health tools could be digital therapeutics. For example, using the medium of virtual reality presents an opportunity to rethink interventions for behavioral health.
- Successfully reimagining care delivery requires a partnership between healthcare stakeholders. Digital health is not separate from “standard” or “traditional” healthcare. Deployed optimally, it is a companion to provider-offered care. Ultimately, for digital health tools to help reimagine and reform healthcare delivery, providers, patients and payors must all be part of that partnership.
- Trust will be imperative for digital health adoption. The relationship between a good healthcare provider and a patient is ultimately personal and built on trust. Additional effort to establish an effective provider-patient relationship without personal contact because of the virtual nature of telehealth is imperative. Digital health adoption also needs to be based on trust and a commitment to care.


